After years of traveling abroad for work, I found myself grounded last year, brought home to Southern California not out of nostalgia but out of necessity. My sister and I made the life-altering decision to purchase a single-story house for our ailing, octogenarian parents after recognizing that they could no longer care for each other. My father had multiple physical ailments, while my mother was gradually slipping away due to Alzheimer’s.
My brother moved in, and my sister, a nurse, visits from the Bay Area one week a month. Since my father died earlier this year, my siblings and I have taken turns caring for my mother, meticulously coordinating our schedules to also accommodate work and personal commitments. We went from being successful professionals in our fields to becoming round-the-clock caregivers in our late 50s.
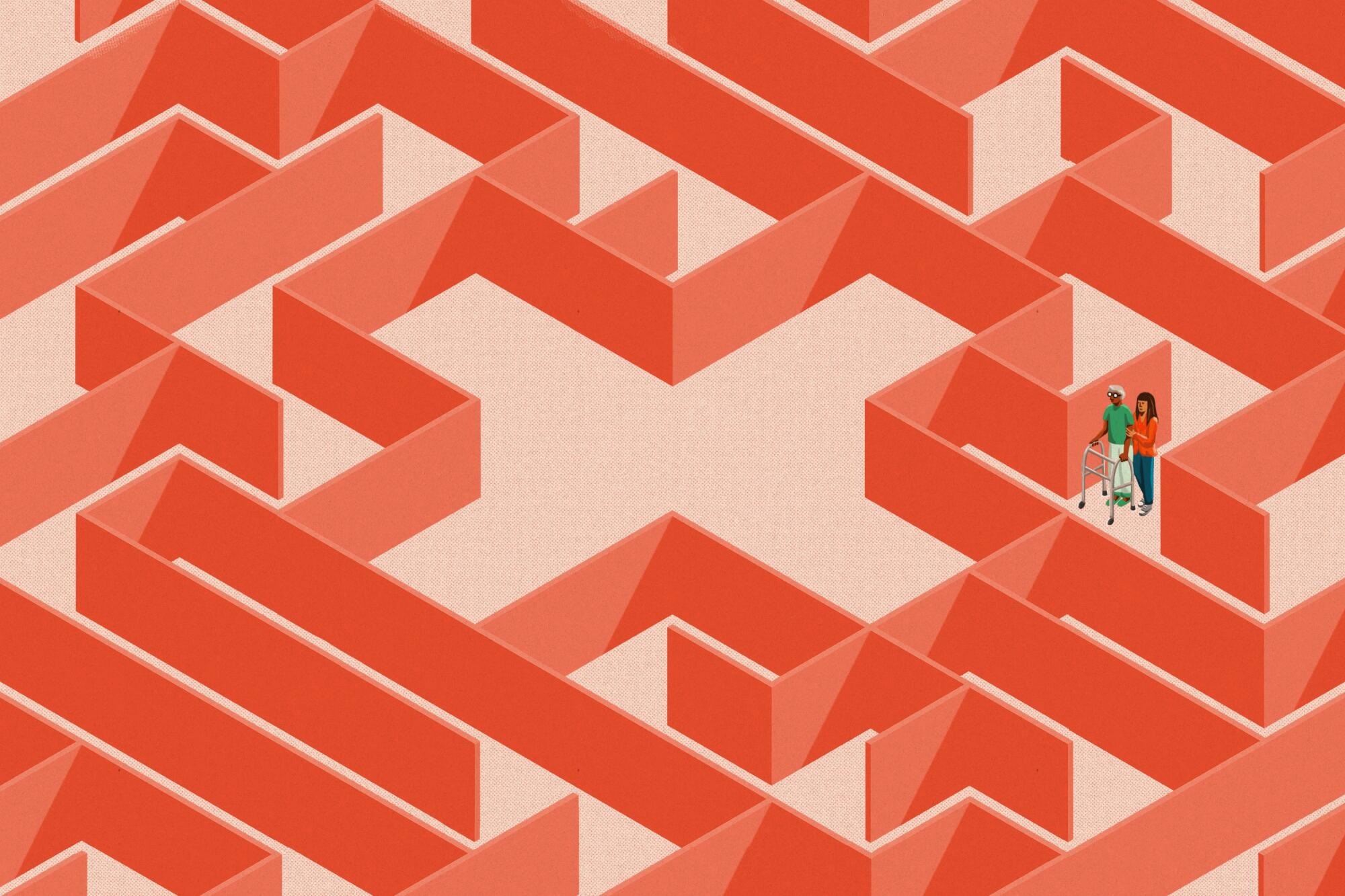
My siblings and I are just a few of the estimated 38 million unpaid caregivers in the United States. We are part of a larger American and global cohort affected by the dramatic aging of the population, the inadequate patchwork of public and private services, and modern migration patterns driven by caregiving.
My 65-year-old mother was working as a nurse until a brain tumor took away almost everything. The sudden life changes that come with caregiving cannot be anticipated.
Like many people in our situation, we found that our parents, once the pillars of our family, suddenly relied on us for their very existence. We feel critically ill-equipped for a huge responsibility that is taking an immense toll on our mental and emotional well-being. Despite being in the company of countless others facing similar challenges in our generation, we have an overwhelming sense of aloneness. Caregivers often grapple with a loss of identity, strained relationships and scarcity of time to rest and recreate
Over the past century, global life expectancy has doubled. Every day, some 10,000 baby boomers turn 65, and by 2040, the number of Americans 85 and older will have doubled in less than two decades. But disparities persist along demographic and economic lines: White Americans tend to live longer than people of color, women outlive men, and the richest percentile of men enjoys 15 more years of life on average than the poorest.
Women, who live longer but have faced historical economic disenfranchisement, often end up on the brink of poverty in their later years; for many, their children are their last hope. My mother would have faced a grim fate if not for me and my siblings.
I was filled with guilt and resentment for what I had to take on. But over time, a community of caregivers helped me find fulfillment.
Children, particularly daughters, often bear the brunt of elder care, child care and other domestic responsibilities within families and worldwide. Many are forced to leave their careers to manage these overwhelming responsibilities.
Bureau of Labor Statistics data indicate particularly high demand for one category of caregivers: home health and personal care aides. Many elderly people and their families would prefer that they age at home, driving demand for people who can care for them there. These jobs are expected to become available at an average rate of more than 700,000 a year to meet the unprecedented growth of the senior population. The American Immigration Council has predicted that by 2031, it will be the country’s largest occupation.
Unfortunately, while the demand is growing, the workforce is shrinking. More than 600,000 such workers are expected to leave their positions this decade for various reasons. The field suffers from high turnover due to low wages, high stress and frequent physical injury compared with other occupations. Gov. Gavin Newsom recently vetoed a bill to apply workplace safety standards to household workers.
Immigrants fill a disproportionate share of these jobs, accounting for 36.5% of those providing home care services as of 2019. My family and culture are part of this global pattern. Caregiving is part of our national identity as Filipinos.
Instead of busing migrants and doing other stunts, why don’t politicians look to the past for policy ideas that could improve our asylum and work permit systems?
Caregivers are among the Philippines’ top exports to the United States and beyond. As of 2019, nearly 200,000 Filipino nurses were working abroad. Other developing regions exporting caregivers include Central and South America, South Asia, and East and West Africa.
The reasons for such migration elude many Americans. Terms like “chain migration” depict immigrants as a burden. In reality, they play a pivotal role in sustaining our extended families. Our reliance on migration for caregiving is both intimate and vital but also poorly understood and ultimately unsustainable in its current form.
The global economics of caregiving are, as my family has discovered, challenging. We explored the possibility of petitioning for my niece, a trained caregiver, to come to the U.S. to help. As part of that process, the U.S. Department of Labor reviewed our job description and set the prevailing wage at $14 an hour. While we’re hurtling toward a future with lots more home healthcare jobs, they’re not currently good jobs.
Case in point: While we would have been required only to pay California’s minimum wage of $15.50 an hour, the living wage for a single adult in San Bernardino County has been estimated at $18.86. For someone like my mother requiring round-the-clock care, $18.86 an hour amounts to $165,000 a year, a burden few can bear.
Social Security, Medicaid, long-term care insurance and other available means of assistance remain woefully insufficient. Long-term care insurance is typically expensive and inadequate. The average monthly Social Security check is about $1,700. Medicaid can cover nursing home care if one qualifies, but my mother and many others don’t. And in California, nursing homes cost more than $9,000 a month on average, while assisted living facilities typically cost $5,000 to $7,000 monthly.
The 2018 RAISE (Recognize, Assist, Include, Support and Engage) Family Caregivers Act directed the U.S. Department of Health and Human Services to develop a national strategy to provide training and resources, financial and workplace support, and respite for caregivers. But it didn’t address the unmet demand for home health aides.
My siblings and I have discovered that despite making significant life changes and financial investments, conducting thorough research, and accessing public and private support for caregivers, we still lack the resources we need to provide my mother with the dignity, loving care and safety she deserves after 81 years on this planet, over 40 of them as a nurse. Placing her in a facility, especially after she lost her husband of 59 years, doesn’t seem like an option in our culture. Hiring home health and personal care aides looks like our only choice.
How can we meet the growing demand for these workers? To start, immigration policies should be reformed. The State Department’s cap on visas for workers deemed unskilled, including healthcare aides, is far too low. A special expedited visa could be established for foreign home health aides, including the undocumented health workers already here. The government could extend the guest worker visa program for agricultural workers to include them.
Additionally, home health aides need living wages to support themselves and their families. And unpaid family caregivers need financial and respite support to navigate the long, exhausting and costly challenges they often face. Only government subsidies are likely to make that possible.
To help all Americans age with grace, we have to recognize and support the vital contributions of the immigrants, families and other caretakers who can literally save our lives.
Gemma Bulos is a social entrepreneur, educator and Public Voices Fellow on Advancing the Rights of Women and Girls with the OpEd Project and Equality Now.
A cure for the common opinion
Get thought-provoking perspectives with our weekly newsletter.
You may occasionally receive promotional content from the Los Angeles Times.






